There is a critical need for additional pain management options that are safer and less habit-forming than opioids. Research shows that cannabis can effectively manage pain with less risk and mitigate much of the danger presented by opioid-based drugs, or opiates. A thorough list of resources is provided at the end of this article.
Chronic Pain and the Opioid Crisis
An estimated one in five US adults suffers from a chronic pain condition lasting over six months and requiring medical treatment. Nearly half of these patients report that their pain persists despite the use of conventional pain medicines, such as NSAIDS and opioids. Many physicians report dissatisfaction with currently available pain treatments. Health economists estimate that the annual cost of chronic pain in the United States is $635 billion in health care costs and lost productivity.
Prescriptions for opioids rose exponentially in the late 1990s and have leveled off in recent years, although they still harm people nationwide. Specifically, the use of hydrocodone doubled while the use of oxycodone increased more than fivefold. These rises in use accompanied an estimated five-fold increase in opioid-related mortality from 1999 to 2017. During that time almost 218,000 people died in the United States from overdoses. In 2017, among 70,237 drug overdose deaths, 47,600 (67.8%) involved opioids. Most telling, however, is that even as the rate of prescriptions for opioids dramatically increased, the percentage of Americans reporting suffering from untreated pain remains largely unchanged.

Can cannabis treat pain and mitigate the opioid crisis? Stock photo.
Cannabis for Pain Relief: The Evidence
Historical references documenting the use of cannabis for therapeutic purposes date back 10,000 years. It was initially recognized in the US Pharmacopoeia in 1850. Early case-series from this time period document the use of cannabis to address pain-related conditions, such as migraine, neuropathy, and musculoskeletal pain. Cannabis-based oral extracts were used widely in the United States throughout the 19th and 20th centuries. Cannabis was removed from the US Pharmacopoeia in 1942 as a direct result of the federal government’s enactment of cannabis prohibition in 1937.
Today there remains significant interest in the utility of cannabis in the treatment of chronic pain. A 2017 literature review identified 35 controlled studies, involving over 2,000 subjects assessing the safety and efficacy of cannabinoids in pain management. More recently, a review of over 10,000 peer-reviewed scientific papers by the National Academies of Sciences, Engineering, and Medicine acknowledged, “There is conclusive or substantial evidence that cannabis is effective for the treatment of chronic pain in adults.” Among chronic pain conditions, cannabis appears most effective for neuropathy, which is a type of nerve-related pain often associated with diabetes, multiple sclerosis, and spinal cord injury. In clinical trials, doses of both low-THC and high-THC varieties of cannabis show efficacy as a pain reliever. Specific flavonoids (phytonutrients) in the cannabis plant also possess significant pain-relieving properties.
Cannabinoids and Opioid Synergy
The co-administration of cannabinoids enhances the analgesic effects of opioids in animal models and human experimental models. In a rat model, the administration of THC concurrently with oxycodone produces greater analgesic effects than the administration of either substance alone. Researchers concluded, “Together these data demonstrate the additive effects of THC and oxycodone and suggest the potential use of THC to enhance therapeutic efficacy, and to reduce the abuse of opioids.” In a clinical model, vaporized cannabis has similarly been shown to act synergistically with opioids, augmenting the pain-relieving activity of morphine and oxycodone in chronic pain subjects and potentially allowing “for opioid treatment at lower doses with fewer side effects.”
Investigators at Columbia University assessed the efficacy of inhaled cannabis and low doses of oxycodone on experimentally induced pain in a double-blind, placebo-controlled model. Researchers assessed subjects’ pain tolerance after receiving both substances separately or in concert with one another. While neither the administration of cannabis nor oxycodone alone significantly mitigated subjects’ pain, the combined administration of both drugs did so effectively. Authors concluded, “Smoked cannabis combined with an ineffective analgesic dose of oxycodone produced analgesia comparable to an effective opioid analgesic dose without significantly increasing cannabis’s abuse liability.
These data substantiate patients’ self-reporting that adjunctive cannabis therapy is associated with a mitigation in their use of opioid pain relievers.

Can cannabis treat pain and mitigate the opioid crisis? Stock photo.
Prevalence of Cannabis Use for Chronic Pain
Pain is the most commonly reported indication for which patients report using medicinal cannabis. According to a 2019 pooled analysis of 15 studies involving over 6,600 medical cannabis patients in over 30 countries, 64 percent of subjects reported using cannabis for pain mitigation.
According to a 2021 analysis of over 61,000 patients seeking medical cannabis recommendations from evaluators in 12 states, chronic pain was the most commonly reported symptom possessed by those requesting cannabis therapy. Among patients enrolled in state-specific medical cannabis access programs, over 65 percent are registered to use the substance for the treatment of chronic pain. It is the most commonly reported qualifying condition among active cardholders. In non-medical states, the majority of patients self-reporting using cannabis therapeutically also report doing so to address chronic pain conditions.
Can cannabis treat pain and mitigate the opioid crisis? Stock photo.
Safety Profile: Cannabis vs. Opioids
Cannabis is not innocuous. Its active constituents produce a variety of physiological and mood-altering effects. More frequently reported effects include drowsiness, dry mouth, redness of the eyes, alteration of time perception, tachycardia (more common in naive users), and dysphoria (typically a result of higher THC consumption). Patients with a family history of psychiatric disorders or cardiovascular risks may be at greater risk of experiencing more significant adverse events, such as psychosis or stroke. However, reports of such severe effects are atypical in patients administered medicinal cannabis in clinical trial settings. In a review of 23 randomized clinical trials assessing the safety of cannabinoids, 97 percent of the side effects reported by patient subjects were categorized as “not serious.” In one long-term trial, chronic pain patients registered to use medical cannabis reported no higher rate of adverse events over a year compared to controls (those pain patients who did not use cannabis). In another study, elderly subjects who consumed medical cannabis for chronic pain over a year exhibited no differences in overall cognitive performance compared to similarly matched non-users.
In some rare cases, cannabinoids may be contraindicated with other conventional medications. Like with any therapeutic agent, patients should consult thoroughly with their physician before deciding whether the medical use of cannabis is safe and appropriate for their specific circumstances.
Cannabis possesses a preferable safety profile compared to that of opioids. Opioids possess a far greater overall risk of addiction and dependence than does cannabis. Specifically, experts estimate that approximately one in 11 subjects exposed to cannabis exhibit symptoms of dependence—a percentage that is only slightly higher than the liability associated with caffeine. This risk may be higher in certain sub-populations, such as those who use cannabis daily or who initiate their use during adolescence. Opioids are also associated with more severe physical symptoms of withdrawal (such as muscle cramping) than is cannabis. Patients taking opioids for pain also often tend to rapidly develop tolerance to the drug, requiring larger doses to maintain the same pain relief. Depression, sedation, constipation, nausea, vomiting, seizures, and other adverse effects may also be associated with opioid use. A 2017 study reported that “levels of depression and anxiety are higher among chronic pain patients receiving prescription opioids compared to those receiving medical marijuana.”
Unlike opioids, cannabinoids are incapable of causing lethal overdose regardless of quantity or potency. The National Cancer Institute states, “Because cannabinoid receptors, unlike opioid receptors, are not located in the brain stem areas controlling respiration, lethal overdoses from cannabis and cannabinoids do not occur.” A 2017 US Drug Enforcement Administration publication affirms, “No deaths from overdose of marijuana have been reported.” For these reasons, the DEA’s own administrative law judge once determined, “Marijuana, in its natural form, is one of the safest therapeutically active substances known to man.” Currently, some experts now opine that physicians, in jurisdictions where medical cannabis is legal, consider cannabis therapy “prior to using opioids” for qualifying pain patients.
Cannabis Substitution Effect
Many ecological trials have assessed whether the enactment of medical cannabis access laws is associated with changes in opioid use behaviors among the general population. The majority of these studies, though not all of them, have identified an association between medical cannabis dispensing and a measurable reduction in opioid use and misuse. However, because of the observational design of such studies, such trends may only be defined as correlative rather than causal. Relevant studies include:
- “Medical marijuana legalization was associated with 23 percent and 13 percent reductions in hospitalizations related to opioid dependence or abuse and opioid-related overdose respectively.” — Shi. 2017.
- “In short, our findings that legally protected and operating medical marijuana dispensaries reduce opioid-related harms suggests that some individuals may be substituting towards marijuana, reducing the quantity of opioids they consume or forgoing initiation of opiates altogether.” — Powell et al.
- “We found that statewide medical cannabis legalization implemented in 1993–2014 in the US was associated with close to 30 percent reductions in Schedule III opioids received by Medicaid enrollees.” —Liang et al.
- ”We examine the association between opioid prescription patterns in privately insured adults and changes in state cannabis laws among five age groups … [I]n states which implemented medical cannabis use laws (but not other categories of cannabis liberalization laws), lower rates of opioid prescription were seen in the younger age cohorts.” — Raji et al. 2019.
- “We use a difference‐in‐difference approach to estimate the effect of medical marijuana laws (MML) and recreational marijuana laws (RML) on fatalities from opioid overdoses, and we find that marijuana access induces sharp reductions in opioid mortality rates. … In our preferred econometric specification, we estimate that RMLs reduce annual opioid mortality in the range of 20–35%, with particularly pronounced effects for synthetic opioids.” — Chan, et al. 2019.
- “Results provide evidence that MMLs may be effective at reducing opioid reliance as survey respondents living in states with medical cannabis legislation are much less apt to report using opioid analgesics than people living in states without such laws.” — Flexon et al., 2019.
- “There was a larger reduction from 2012 to 2017 in Colorado (-31.5%) than the other states. Colorado had a significantly greater decrease in codeine and oxymorphone than the comparison states.” — Lopez et al., 2020.
- “In this study, we observed an association between state-level legalization of medical cannabis and opioid prescribing by orthopedic surgeons in the Medicare Part D cohort. We found that overall opioid prescribing by orthopedic surgeons in this cohort was reduced in states permitting patient access to medical cannabis, compared with those who do not.” — Lopez et al., 2020.
- “Increased medical and recreational storefront dispensary counts [in the United States] are associated with reduced opioid related mortality rates during the study period. These associations appear particularly strong for deaths related to synthetic opioids such as fentanyl.” — Hou et al., 2020.
A widely publicized 2014 study in the journal JAMA Internal Medicine reported that the passage of medical cannabis laws between the years 1999 and 2010 was associated with “significantly lower state-level opioid overdose mortality rates” (up to 33 percent). However, a follow-up study using similar methods reported that these trends were not sustained long term, and ultimately the trend reversed over time (through 2017).
More recently, an analysis of approximately 800,000 urine drug test results collected from pain management patients between the years 2016 and 2018 reported that those samples that tested positive for cannabis use were less likely to possess high concentrations of opioids. Investigators reported that “for each of the eight opioids monitored, lower mean concentrations were observed when THC-COOH was also present in the sample. … The largest shift was seen in codeine positive samples, followed by morphine, and fentanyl.” Although authors cautioned that the observational design of the study precluded them from “assigning causation” to their results, they did acknowledge that the findings were “consistent with data from self-report surveys of medical cannabis patients” in which subjects frequently report substituting cannabis for opioids.
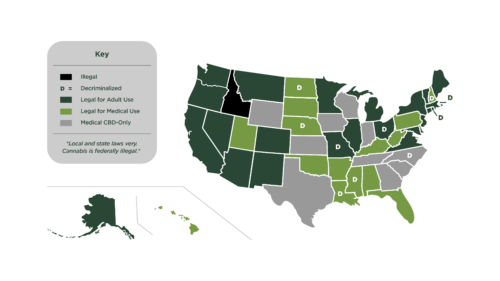
Legalization map 2024. Copyright Oaksterdam University.
Patient Population Data
In addition to ecological studies, numerous retrospective and longitudinal studies have assessed opioid use trends in specific patient populations following their initiation of medical cannabis therapy. In contrast to observational, population-based studies, which only seek to identify whether an association exists between the passage of medical cannabis laws and opioid use trends in the general population, this data explicitly assesses whether cannabis access influences individuals’ behavior. Many of these studies provide persuasive evidence that patients diagnosed with chronic pain and other debilitating conditions typically reduce, or in some cases, eliminate their use of opioids following their enrollment in sanctioned cannabis access programs. These include data from the following jurisdictions:
- Arizona: “Patients reported using medical cannabis to treat a variety of conditions. … [P]atients reported using other medications less frequently when using cannabis. This is consistent with findings from other studies.”
- Illinois: “[O]ur results indicate that MC (medical cannabis) may be used intentionally to taper off prescription medications. These findings align with previous research that has reported substitution or alternative use of cannabis for prescription pain medications due to concerns regarding addiction and better side-effect and symptom management, as well as complementary use to help manage side-effects of prescription medication.”
- Michigan: “Among study participants, medical cannabis use was associated with a 64 percent decrease in opioid use, decreased number and side effects of medications, and an improved quality of life. … This study suggests that many chronic pain patients are essentially substituting medical cannabis for opioids and other medications for chronic pain treatment, and finding the benefit and side effect profile of cannabis to be greater than these other classes of medications.”
- Minnesota: “Over the course of this 6-month retrospective study, patients using medical cannabis for intractable pain may have experienced a significant reduction in the average MME (milligram morphine equivalents) available for pain control. A non–statistically significant difference in average benzodiazepine dose was observed. The results of this study add to the currently mixed body of evidence suggesting that medical cannabis may be effective for treating pain.”
- New Mexico: Compared to non-users, medical cannabis enrollees “were more likely either to reduce daily opioid prescription dosages between the beginning and end of the sample period (83.8 versus 44.8 percent) or to cease filling opioid prescriptions altogether (40.5 versus 3.4 percent). … The clinically and statistically significant evidence of an association between MCP (medical cannabis program) enrollment and opioid prescription cessation and reductions and improved quality of life warrants further investigations on cannabis as a potential alternative to prescription opioids for treating chronic pain.”
- New York: “After three months [of] treatment, medical cannabis improved [subjects’] quality of life, reduced pain and opioid use, and led to cost savings.”
- Canada: “A 239-question cross-sectional survey was sent out via email in January 2017 to gather comprehensive information on cannabis use from Canadian medical cannabis patients registered with a federally authorized licensed cannabis producer, resulting in 2032 complete surveys. … The most commonly cited substitution was for prescription drugs (69.1 percent), followed by alcohol (44.5 percent), tobacco (31.1 percent), and illicit substances (26.6 percent). … Of the 610 mentions of opioid medications, participants self-reported they stopped using 59.3 percent completely (100 percent substitution), and a further 18.4 percent reduced their use by 75 percent.”
In 2019, Canadian and US researchers published the results of a longitudinal study assessing drug use trends in chronic pain patients over a multi-year period. Authors reported “an independent negative association between frequent cannabis use and frequent illicit opioid use.” Specifically, subjects who consumed cannabis daily “had about 50 percent lower odds of using illicit opioids every day [as] compared to cannabis non-users.” Authors concluded, “These findings provide longitudinal observational evidence that cannabis may serve as an adjunct to or substitute for illicit opioid use among PWUD (people who use drugs) with chronic pain.”
Similarly, a 2020 Israeli study of chronic pain patients prescribed medical cannabis reported a “decrease of 42 percent from baseline in morphine equivalent daily dosage of opioids” over one year. In yet another longitudinal study, scientists studied the influence of medical cannabis use on opioid patterns in pain patients over a year. They reported: “In patients who reported opioid medication use at baseline, there were significant reductions in oral morphine equivalent doses. … Taken together, the results of this study add to the cumulative evidence in support of plant-based medical cannabis as a safe and effective treatment option and potential opioid substitute or augmentation therapy for the management of chronic pain symptomatology and quality of life.”
Longitudinal data collected over 12 months in Canada show that authorized medical cannabis patients who suffer from chronic pain conditions “significantly” reduce their opioid use long-term. Over the study period, “The proportion of individuals who reported using opioids decreased by half,” researchers determined. They added that subjects’ “pain intensity and pain-related interference scores were reduced and [their] quality of life and general health symptom scores were improved compared with baseline. … [B]eneficial effects of cannabis appear to persist long-term and tolerance may not become a significant issue for patients on a stable regimen.”
Longitudinal assessments of opioid use patterns in other patient populations, such as cancer patients, similarly show reductions in opioid consumption following the initiation of cannabis therapy.

Can cannabis treat pain and mitigate the opioid crisis? Stock photo.
Cannabis, Pain, Opioids, and Cravings
The question of whether cannabinoids may reduce specific drug cravings and/or ease specific symptoms of substance abuse withdrawal has been the subject of less scientific scrutiny. However, initial data shows some promising, though far from definitive, results.
For example, a pair of clinical studies reported an association between cannabis use and decreased use of crack cocaine. In a clinical trial, the administration of the compound CBD was shown to reduce subjects’ cravings for tobacco. CBD administration was demonstrated in another clinical trial to reduce cue-induced cravings and anxiety in subjects with a history of heroin use.
In a 2020 case-control study, subjects administered oral THC experienced a ninefold reduction in opioid consumption as compared to those who were not administered the substance. Similar results have been identified in animal models, leading some experts to suggest that “cannabis may play a role in ameliorating the impact of opioid use disorder. … Adjunct cannabis use alongside current treatment strategies could help to improve the number of individuals engaging in OUD (opioid use disorder) treatment, as well as increase treatment retention rates.”
A 2018 study further reported that “individuals initiating OAT (opioid agonist treatment) were approximately 21 percent more likely to be retained in treatment at six months if they reported daily use of cannabis,” while another study demonstrated that the use of oral THC “reduced the severity of opiate withdrawal during acute detoxification.” These data indicate the potential role for either the adjunctive use of cannabinoids or cannabinoid agonists in improving treatment outcomes in certain substance abuse dependent subjects.
Cannabis as a Pain and Harm Reduction Agent in the Opioid Crisis
Cannabis ought not to be viewed as a silver bullet solution to the opioid crisis, nor should it be seen as a blanket replacement for opioid analgesics. However, cannabinoids often possess a preferable side-effect profile compared to opioids, and a growing body of data supports their potential use as an adjunctive treatment in some pain patients which may ultimately lead to the reduction or elimination of the use of some other prescription medications.
Recently published data indicates that many patients are currently using cannabis in such a manner and that it may provide “pharmacological support” to assist them in tapering their use of opioids. Specifically, data compiled in 2019 from a nationally representative sample of pain patients finds, “[S]ubstitution of marijuana for opioids, which included a substantial degree of opioid discontinuation (~20 percent), was common. Our findings are consistent with prior surveys of American and Canadian marijuana users in which substitution of marijuana for opioids was prevalent due to better symptom management and fewer adverse and withdrawal effects. … The impact of marijuana substitution for opioids and concomitant opioid and marijuana use … warrants [further] investigation.”
Data published in 2020 that surveyed over 500 state-authorized medical cannabis patients further affirmed these findings. Authors determined that 45 percent of those surveyed reported decreasing their opioid usage following the initiation of cannabis therapy and another 40 percent of respondents acknowledged ceasing their use of opioids altogether. They concluded: “To our knowledge, this is one of the largest surveys of chronic pain patients who used opioids continuously for a minimum of three months and combined it with medical cannabis. Our results show a remarkable percentage of patients both reporting complete cessation of opioids and decreasing opioid usage by the addition of medical cannabis, with results lasting for over a year for the majority. … We believe our results lend further support that medical cannabis provided in a standardized protocol can lead to decreased pain and opioid usage, improved function, and quality of life measures, and even complete cessation of opioids in patients with chronic pain treated by opioids.”
Most recently, in 2020, a consortium of over 20 physicians authored “consensus-based recommendations surrounding the safe introduction and titration of cannabinoids in concert with tapering opioids.”
References
- Abrams et al., 2011. Cannabinoid-opioid interaction in chronic pain, Clinical Pharmacology and Therapeutics.
- Armentano, 2007. Cannabis, Mental Health and Context. NORML Foundation.
- Aviram et al., 2020. Medical cannabis treatment for chronic pain: Outcomes and predictions. European Journal of Pain.
- Bachhuber et al., 2014. Medical cannabis laws and opioid analgesic overdose mortality in the United States, 1999-2010. JAMA Internal Medicine.
- Baron. 2018. Medicinal properties of cannabinoids, terpenes, and flavonoids in cannabis, and benefits in migraine, headache, and pain: An update on current evidence and cannabis science. Headache.
- Bellneir et al., 2018. Preliminary evaluation of the efficacy, safety, and costs associated with the treatment of chronic pain with medical cannabis. Mental Health Clinician.
- Bisaga et al., 201518. The effects of dronabinol during detoxification and the initiation of treatment with extended release naltrexone. Drug and Alcohol Dependence.
- Boehnke et al., 2016. Medical cannabis use is associated with decreased opiate medication in a retrospective cross-sectional survey of patients with chronic pain. Journal of Pain.
- Boehnke et al., 2019. Qualifying conditions of medical cannabis license holders in the United States, Health Affairs.
- Bruce et al., 2018. Preferences for medical marijuana over prescription medications among persons living with chronic conditions: Alternative, complementary, and tapering uses. Journal of Alternative and Complementary Medicine.
- Cannabis and Cannabinoids PDQ, 2019.
- Center for Disease Control and Prevention, “Prescription Opioid Data.”
- Chami and Kim. 2019. Cannabis use and elevated risk of myocardial infarction in the young: A population-based study. Mayo Clinic Proceedings.
- Chan et al., 2019. The effects of recreational marijuana legalization and dispensing on opioid mortality. Economic Inquiry.
- Dranitsaris et al., 2021. Opioid-prescribing in Canada following the legalization of cannabis: A clinical and economic time-series analysis. Applied Health Economics and Health Policy.
- Feingold et al., 2017. Depression and anxiety among chronic pain patients receiving prescription opioids and medical marijuana. Journal of Affective Disorders.
- Flexon et al., 2019. The effect of cannabis laws on opioid use. International Journal of Drug Policy.
- Goggins et al., 2019. Reduced opioid levels from pain management patients associated with marijuana use. Pain Management.
- Grotenhermen and Muller-Vahl. 2017. Medicinal uses of marijuana and cannabinoids, Critical Reviews in Plant Sciences.
- “History of Cannabis as a Medicine: Nineteenth Century Irish Physicians and Correlations of Their Observations to Modern Research,” in Cannabis Sativa L – Botany and Biotechnology, 2017.
- Hou et al., 2020. Association between county level cannabis dispensary counts and opioid related mortality rates in the United States: panel data study. BMJ.
- Hsu and Painter, 2019. Probable interaction between Warfarin and inhaled and oral administration of cannabis, Journal of Pharmacy Practice.
- Ishida et al. 2019. Substitution of marijuana for opioids in a national survey of US adults. PLOS One.
- Khan et al., 2019. Perspectives on cannabis as a substitute for opioid analgesics. Pain Management.
- Kosiba et al., 2019. Patient-reported use of medical cannabis for pain, anxiety, and depression symptoms: Systematic review and meta-analysis, Social Science & Medicine.
- Labigalini et al., 1999. Therapeutic use of cannabis by crack addicts in Brazil. Journal of Psychoactive Drugs.
- Lake et al., 2019. Frequency of cannabis and illicit opioid use among people who use drugs and report chronic pain: A longitudinal analysis. PLOS One.
- Liang et al., 2018. Medical cannabis legalization and opioid prescriptions: Evidence on US Medicaid enrollees during 1993-2014. Addiction.
- Lopez et al., 2020. State medical cannabis laws associated with reductions in opioid prescriptions by orthopaedic surgeons in Medicare Part D cohort. Journal of the Academy of Orthopaedic Surgeons.
- Lopez et al., 2020. Prescription opioid distribution after the legalization of recreational marijuana in Colorado. International Journal of Research and Public Health.
- Lucas et al., 2019. Medical cannabis patterns of use and substitution for opioids & other pharmaceutical drugs, alcohol, tobacco, and illicit substances; results from a cross-sectional survey of authorized patients. Harm Reduction Journal.
- Lynch and Campbell. 2011. Cannabinoids for treatment of chronic non-cancer pain: A systematic review of randomized trials, British Journal of Clinical Pharmacology.
- Mahabir et al., 2021. Medical cannabis use in the United States: A retrospective database study. Journal of Cannabis Research.
- McBrien et al, 2019. Cannabis use during methadone maintenance for opioid use disorder: A scientific review and meta-analysis. CMAJ.
- Medical Express, July 24, 2019, “Researchers unlock access to pain relief potential of cannabis.”
- Meng et al., 2021. Patient-reported outcomes in those consuming medical cannabis: A prospective longitudinal observational study in chronic pain patients. Canadian Journal of Anaesthesia.
- Morgan et al. 2013. Cannabidiol reduces cigarette consumption in tobacco smokers: preliminary findings. Addictive Behaviors.
- National Academy of Sciences, Engineering, and Medicine. The Health Effects of Cannabis and Cannabinoids: Report Conclusions, 2017.
- Nguyen et al., 2019. Delta-9-THC attenuates oxycodone self-administration under extended access conditions, Neuropharmacology.
- NORML. Emerging Clinical Applications for Cannabis & Cannabinoids.
- NORML v DEA, In the Matter of Marijuana Rescheduling, 1988.
- O’Connell et al., 2019. Medical cannabis: Effects on opioids and benzodiazepine requirements for pain control. The Annals of Pharmacotherapy.
- Pawasarat et al., 2020. The efficacy of medical marijuana in the treatment of cancer-related pain. Journal of Palliative Medicine.
- Powell et al., 2018. Do medical marijuana laws reduce addictions and deaths related to pain killers? Journal of Health Economics.
- Raji et al. 2019. Association between cannabis laws and opioid prescriptions among privately insured adults in the US, Preventive Medicine.
- Rod, Kevin, 2019. A pilot study of a medical cannabis — opioid reduction program. The American Journal of Psychiatry and Neuroscience.
- Safakish et al., 2020. Medical cannabis for the management of pain and quality of life in chronic pain patients: A prospective observational survey. Pain Medicine.
- Schneider-Smith et al., 2020. Matched pilot study examining cannabis-based dronabinol for acute pain following traumatic injury. Trauma Surgery and Acute Care Open.
- Science Daily, September 11, 2012, “Chronic pain costs the U.S. up to $635 billion, study shows.”
- Shah et al., 2020. Association of marijuana use and cardiovascular disease: A behavioral risk factor surveillance system risk factor analysis of 133,706 US adults. The American Journal of Medicine.
- Shi. 2017. Medical marijuana policies and hospitalizations related to marijuana and opioid pain relievers. Drug and Alcohol Dependence.
- Sihota et al., 2020. Consensus-based recommendations for titrating cannabinoids and tapering opioids for chronic pain control. International Journal of Clinical Practice.
- Shover et al., 2019. Association between medical cannabis laws and opioid overdose mortality has reversed over time. PNAS.
- Socias et al., 2017. Intentional cannabis use to reduce crack cocaine use in a Canadian setting: A longitudinal analysis. Addictive Behaviors.
- Socias et al., 2018. High-intensity cannabis use is associated with retention in opioid agonist treatment: a longitudinal analysis. Addiction.
- Sznitman et al., 2020. Medical cannabis and cognitive performance in middle to old adults treated for chronic pain. Drug and Alcohol Review.
- Takakuwa and Sulak. 2020. A survey on the effect that medical cannabis has on prescription opioid medication usage for the treatment of chronic pain at three medical cannabis practice sites. Cureus.
- The Cannabist, July 12, 2017, “Even the DEA says nobody has ever died of a marijuana overdose.”
- “Trends in Opioid Use, Harms, and Treatment,” in Pain Management and the Opioid Epidemic, 2017.
- Troutt and DiDonato. 2015. Medical cannabis in Arizona: Patient characteristics, perceptions, and impressions of medical cannabis legalization, Journal of Psychoactive Drugs.
- US National Library of Medicine, Opioid addiction.
- Vigil et al., 2017. Associations between medical cannabis and prescription opioid use in chronic pain patients: A preliminary cohort study. PLOS ONE.
- Wang et al., 2008. Adverse effects of medicinal cannabinoids, Canadian Medical Association Journal.
- Ware et al., 2015. Cannabis for the management of pain: Assessment of safety study, Journal of Pain.
- Webster et al., 2020. Prescribed medical cannabis in women with gynecological malignancies: A single-institution survey-based study. Gynecologic Oncology Reports.
- Wiese and Wilson-Poe. 2018. Emerging evidence for cannabis’ role in opioid use disorder. Cannabis and Cannabinoid Research.
